Infertility Testing
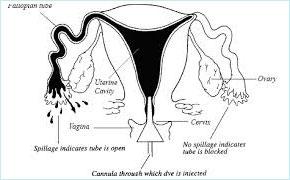 1. A hysterosalpingogram or HSG is an x-ray procedure performed to determine whether the fallopian tubes are patent (open) and to see if the shape of the uterine cavity is normal. An HSG is an outpatient procedure that usually takes less than 30 minutes to perform. It is usually done after the menstral period has ended, but before ovulation, to prevent interference with potential pregnancies.
1. A hysterosalpingogram or HSG is an x-ray procedure performed to determine whether the fallopian tubes are patent (open) and to see if the shape of the uterine cavity is normal. An HSG is an outpatient procedure that usually takes less than 30 minutes to perform. It is usually done after the menstral period has ended, but before ovulation, to prevent interference with potential pregnancies.
How is a hysterosalpingogram done?
A woman is positioned under a fluoroscope (a real-time x-ray imager) on a table. The gynecologist or radiologist then examines her uterus and places a speculum in her vagina. Her cervix is cleaned, and a device (cannula) is placed into the opening of the cervix. The doctor then gently fills the uterus with a liquid containing iodine (contrast) through the cannula. The contrast then enters the tubes, outlines the length of the tubes, and spills out their ends if they are open. Also abnormalities within the uterine cavity may be detected by the doctor observing the x-ray images. The HSG procedure is not designed to evaluate the ovaries or diagnose endometriosis. Frequently, side views of the uterus and tubes are obtained by having the woman change her position on the table. After the HSG, a woman can immediately resume normal activities, although some doctors ask that she refrain from intercourse for a few days.
Is it uncomfortable?
An HSG usually causes mild or moderate uterine cramping for about five to ten minutes however, some women may experience cramps for several hours. The symptoms can be greatly reduced by taking medications used for menstrual cramps. Women should be prepared to have a family member or friend drive them home after the procedure.
Does a hysterosalpingogram enhance fertility?
It is controversial whether this procedure enhances fertility. Some studies indicate a slight increase in fertility lasting about three months after a normal HSG. Most doctors perform the HSG only for diagnostic reasons.
What are the risks and complications of HSG?
• An HSG is considered a very safe procedure. However, there is a set of recognized complications, some serious, which occur less than 1% of the time.
• Infection - The most common serious problem with the HSG is pelvic infection. This usually occurs when a woman has a previous tubal disease. In rare cases, infection can damage the fallopian tubes or necessitate their removal. A woman should call her doctor if she experiences increasing pain or a fever within one to two days of the HSG.
• Fainting - Rarely the woman may get light-headed during or shortly after the procedure.
• Radiation Exposure - Radiation exposure from a HSG is very low, less than with a kidney or bowel study, and there have been no demonstrated ill effects from this radiation, even if conception occurs later the same month. The HSG should not be done if pregnancy is suspected.
• Iodine Allergy - Rarely, a woman may have an allergy to the iodine contrast used in an HSG. A woman should inform her doctor if she is allergic to iodine, intravenous contrast dyes or seafood. Women who are allergic to iodine should have the HSG procedure performed without an iodine containing contrast solution. If a woman experiences a rash, itching, or swelling after the procedure, she should contact her doctor.
• Spotting - Spotting commonly occurs for one to two days after the HSG. Unless instructed otherwise, a woman should notify her doctor if she experiences heavy bleeding after the HSG.
What is the next step if my tubes are blocked?
If your tubes are blocked your doctor will likely recommend either a surgical procedure to directly view the tubes (laparoscopy) or bypass the tubes and perform in vitro fertilization (IVF). This is a complex decision that should be discussed with your doctor.
Are there other options to evaluate tubal patency?
Laparoscopy can also determine either fallopian tubes are open or not, using a procedure called Laparoscopy and dye test. An alternative procedure to evaluate tubal patency is a sonohysterosalpingogram. For this procedure, a catheter (narrow tube) is placed in the uterus through the vagina and saline and air are injected. In women that have open fallopian tubes, tiny air bubbles can be seen going through the fallopian tubes during the ultrasound. Nevertheless, HSG remains the most commonly performed procedure to evaluate tubal patency.
2. Transvaginal Scan
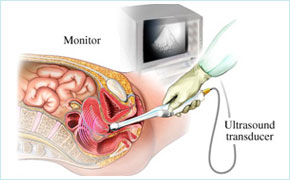 Transvaginal ultrasound is a type of pelvic ultrasound. It is used to look at a woman's reproductive organs, including the uterus, ovaries, cervix, and vagina. Transvaginal means across or through the vagina.
Transvaginal ultrasound is a type of pelvic ultrasound. It is used to look at a woman's reproductive organs, including the uterus, ovaries, cervix, and vagina. Transvaginal means across or through the vagina.
How to Prepare for the Test
You will be asked to undress, usually from the waist down. A transvaginal ultrasound is done with your bladder empty.
How the Test Will Feel
The test is usually painless, although some women may have mild discomfort from the pressure of the probe. Only a small part of the probe is placed into the vagina.
Why the Test is performed
Transvaginal ultrasound may be done for the following problems:
Abnormal findings on a physical exam, such as cysts, fibroid tumors, or other growths, abnormal vaginal bleeding and menstrual problems, Certain types of infertility, Ectopic pregnancy, Pelvic pain.
Risk
There are no known harmful effects of transvaginal ultrasound on humans. Unlike traditional x-rays, there is no radiation exposure with this test.
3. Ovulation detection
Ovulation, the release of an egg from its follicle in one of a woman’s two ovaries, is one of the most important factors in conceiving a child. Ovulation is triggered by a serge of luteinizing hormone (LH) in the woman’s blood, and occurs approximately 36 hours after the start of the LH serge. Because a variety of problems can prevent or disrupt ovulation and result in infertity, often it is necessary to determine whether or not a woman is ovulating. There are several ways to detect ovulation, including urine test kits to measure LH levels, transvaginal ultrasound, endometrial biopsy, blood tests to measure hormone levels, and the basal body temperature (BBT) chart.
Urine Test Kits to Measure Luteininzing Hormone (LH) Levels.
 Several ovulation prediction tests are available at drug stores. These kits use test strips that show changes in the level of LH in the urine. Once the LH serge has occurred, ovulation usually takes place within 12 to 36 hours. Urine testing usually begins two days prior to the expected day of ovulation. For women with 28-day cycles, ovulation usually occurs on days 13 to 15. For women with irregular menstrual cycles, urine testing should be timed according to the earliest and latest possible dates of ovulation. If the cycle ranges between 27 to 34 days, ovulation usually occurs between days 13 to 20. Therefore, testing should begin on day 11 and continue until ovulation is indicated or through day 20. There is an 80% chance of detecting ovulation within five days of testing, and a 95% chance within 10 days of testing. Once ovulation is documented, it is no longer necessary to continue testing during that cycle. Occasionally, ovulation may not occur in a particular cycle. If ovulation is not detected in two or more consecutive cycles, an ovulatory problem may be present.
Several ovulation prediction tests are available at drug stores. These kits use test strips that show changes in the level of LH in the urine. Once the LH serge has occurred, ovulation usually takes place within 12 to 36 hours. Urine testing usually begins two days prior to the expected day of ovulation. For women with 28-day cycles, ovulation usually occurs on days 13 to 15. For women with irregular menstrual cycles, urine testing should be timed according to the earliest and latest possible dates of ovulation. If the cycle ranges between 27 to 34 days, ovulation usually occurs between days 13 to 20. Therefore, testing should begin on day 11 and continue until ovulation is indicated or through day 20. There is an 80% chance of detecting ovulation within five days of testing, and a 95% chance within 10 days of testing. Once ovulation is documented, it is no longer necessary to continue testing during that cycle. Occasionally, ovulation may not occur in a particular cycle. If ovulation is not detected in two or more consecutive cycles, an ovulatory problem may be present.
Transvaginal Ultrasound
Follicular growth can be measured with ultrasound, a technique which uses sound waves to produce an image on a monitor screen. This is a painless procedure usually done with a probe inserted into the vagina, but may be done with an external probe placed on the abdomen. Prior to ovulation, the follicle is thin-walled and filled with fluid. As the egg inside the follicle develops, the follicle increases in size. Ovulation generally occurs when the follicle measures about 1.8 to 2.5 centimeters. Ultrasound may be useful for timing intercourse or insemination. In women taking fertility drugs, ultrasound may be performed on several different days during the menstrual cycle so that each follicle can be measured precisely and monitored.
Blood Tests to Measure Hormone Levels.
Elevated progesterone levels in the blood usually are associated with ovulation. A blood test to measure progesterone can be performed about one week before the anticipated onset of the next menstrual period. The LH surge occurs just before ovulation. LH levels in the blood or urine can be measured to predict when the follicle is mature and ready for ovulation. Estrogen is secreted by the growing follicle and rises rapidly prior to ovulation. If ovulation is being induced with fertility drugs, frequent estrogen level measurements may be needed to determine follicular growth.
Basal Body Temperature (BBT) Chart.
The basal body temperature chart helps to monitor the duration of the different phases of the menstrual cycle, and can help determine if and when ovulation has occurred. During the follicular phase, the woman's body temperature is relatively low. When progesterone production begins at ovulation, it produces a temperature rise with a minimum increase of 0.5 degrees Fahrenheit. An increased body temperature for several days indicates ovulation has occurred. BBT charts cannot predict when ovulation is going to occur; they only confirm that ovulation has occurred after the fact. Some women will monitor changes in their cervical mucus along with their BBT. As ovulation approaches, a woman's cervical mucus becomes more abundant, thin, slippery, and stretchy. This is an inexpensive, natural way to help identify a woman's most fertile days. Although determining if and when ovulation is occurring might seem frustrating and time consuming, it is often an essential step toward achieving pregnancy. It is important that women work with their consultant to decide which method of ovulation detection is best for them. If these tests indicate that the woman is not ovulating, or that she has irregular cycles, treatments are available to correct the problem and increase the chances of a successful pregnancy.
4. Hormonal Profile
FSH,LH,Prolactin-,TFT, Estradiol and AMH are the basic hormone test to evaluate the cause of infertility.
5.Semen analysis
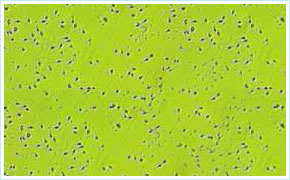 Semen analysis is the microscopic examination of semen (the male ejaculate) to determine its volume, the number of sperm (sperm count), their shapes (morphology), and their ability to move (motility) in addition to other parameters. Semen analysis is the cornerstone of the laboratory evaluation of the infertile male and helps to decline the severity of the male factor. Service provider will provide patients with standardized instructions for semen collection, including a pre-test abstinence interval of two to five days. Although a standard duration of abstinence is important for evaluation of semen parameters, some men with severe oligozospermia can have equal or better sperm concentration with a short (hours) period of abstinence, supporting the potential use of multiple semen analyses during assisted reproductive technology (ART) treatment cycles. Semen can be collected by masturbation into a specimen cup or by intercourse using special semen collection condoms that do not contain substances toxic to sperm. Ideally, the specimen should be collected at the laboratory. If collected at home, the specimen should be kept at room or body temperature during transport and examined in the laboratory within one hour of collection. The semen analysis provides information on semen volume as well as sperm concentration, motility, and morphology.
Semen analysis is the microscopic examination of semen (the male ejaculate) to determine its volume, the number of sperm (sperm count), their shapes (morphology), and their ability to move (motility) in addition to other parameters. Semen analysis is the cornerstone of the laboratory evaluation of the infertile male and helps to decline the severity of the male factor. Service provider will provide patients with standardized instructions for semen collection, including a pre-test abstinence interval of two to five days. Although a standard duration of abstinence is important for evaluation of semen parameters, some men with severe oligozospermia can have equal or better sperm concentration with a short (hours) period of abstinence, supporting the potential use of multiple semen analyses during assisted reproductive technology (ART) treatment cycles. Semen can be collected by masturbation into a specimen cup or by intercourse using special semen collection condoms that do not contain substances toxic to sperm. Ideally, the specimen should be collected at the laboratory. If collected at home, the specimen should be kept at room or body temperature during transport and examined in the laboratory within one hour of collection. The semen analysis provides information on semen volume as well as sperm concentration, motility, and morphology.
6.Basic test
( Infection screening,Blood for complete picture,Blood glucose,Blood grouping and urine for routeine examination,etc;)

