2. Intrauterine insemination (IUI)
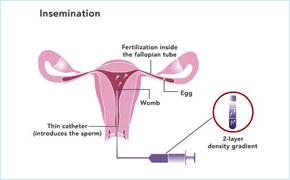 The aim of IUI is to place a small volume of prepared motile sperm high in the uterus on the day of ovulation. It is the way in which best motile sperms are introduced at the right time of the cycle physically closed to the uterus, by passing the cervical mucus. Since the 19th century, there had been reports of pregnancies resulting from the artificial insemination (AI) using neat sperm.
The aim of IUI is to place a small volume of prepared motile sperm high in the uterus on the day of ovulation. It is the way in which best motile sperms are introduced at the right time of the cycle physically closed to the uterus, by passing the cervical mucus. Since the 19th century, there had been reports of pregnancies resulting from the artificial insemination (AI) using neat sperm.
Disadvantage of using neat semen are the risk of infection as well as occurance of painful uterine contractions and even collapse in rare cases. Nowadays, semen preparation methods are developed to select best motile sperm and also to eliminate the chance of infection and pain. This will increase the pregnancy rate compared to neat semen or natural intercourse.
IUI may or may not be combined with ovulation induction or controlled ovarian hyperstimulation (COH). The principal of ovulation induction is to produce more number of eggs by stimulating the ovaries with fertility drugs. Thus, the number of available eggs are increased and chance of conceiving is higher than natural intercourse.
It is also vital that the treatment is monitored properly to measure the growth of follicles by transvaginal ( internal) ultrasound scan at least 2 to 3 times during a treatment cycle. Measuring the hormone level in blood and urine may also be necessary.
SUCCESS RATE
Success rate can be varied from approximately 15% per cycle and cumulative pregnancy rate by 3 cycles is 40% rising to 60% after 6 cycles. In conclusion,IUI is simple but cost effective way of assisted reproduction technique which can be done as out patient without any anesthesia or pain. Followings are groups of patients who can benefit from treatment with IUI;
(1) Anovulatory infertility
(2) Cervical mucus hostility
(3) Mile male factor infertility
(4) Immunological infertility
(5) Unexplained infertility

